Pokushalov及同事假设,在高血压控制不良的患者中,肾动脉去神经术(RAD)可对心房颤动(AF)模式产生有益影响。在一项随机双盲研究中,在有耐药性高血压的AF患者中,比较了在肺静脉隔离(PVI)基础上增加RAD与PVI加药物治疗的疗效。
Pokushalov及同事假设,在高血压控制不良的患者中,肾动脉去神经术(RAD)可对心房颤动(AF)模式产生有益影响。在一项随机双盲研究中,在有耐药性高血压的AF患者中,比较了在肺静脉隔离(PVI)基础上增加RAD与PVI加药物治疗的疗效。1年后,在接受RAD加PVI治疗的患者中观察到收缩压和舒张压的显著降低。12个月时,69%的PVI加RAD组患者无AF,与之相比,仅做PVI组患者中仅29%无AF。这些结果表明,RAD不仅有助于控制高血压,还可能降低AF风险。(图3)
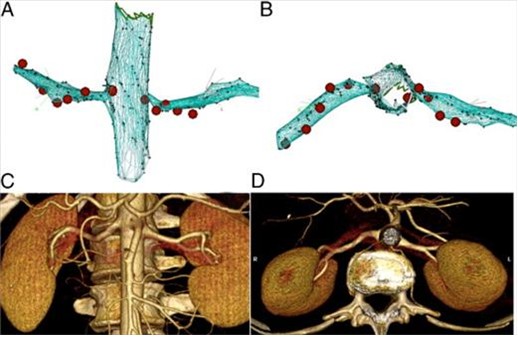
图3 肾脏去神经术射频位点(A,B)和术后6个月时肾动脉磁共振成像(C,D)
J Am Coll Cardiol. 2012;60(13):1163-1170.
点评
The effect of renal denervation in patients with atrial fibrillation
Gavin W Lambert and Markus P Schlaich
澳大利亚Baker IDI Heart & Diabetes Institute
Atrial fibrillation (AF) is the most common presentation of cardiac arrhythmias. The main risk factors for AF incidence are elevated blood pressure, a history of cardiac disease, overweight and obesity, diabetes mellitus and smoking (Circulation 123:1501-1508, 2011). The prevalence of AF increases with age. While in some patients AF may appear relatively benign, the condition is often associated with palpitations, chest pain or discomfort, fainting or dizziness and fatigue. Importantly, AF may be associated with heart failure and is an independent risk factor of stroke. Interestingly, while the effects of other factors such as hypertension, coronary heart disease, and heart failure on the risk of stroke become progressively weaker with aging, this is not the case for AF. While a large proportion of patients with newly diagnosed AF may spontaneously revert to normal rhythm, AF recurrence is common in many of these patients. Pharmacological treatment of persistent AF will typically involve consideration of control of heart rate and/or rhythm and prevention of clot formation. In those patients with drug refractory paroxysmal AF, pulmonary vein isolation is an established therapeutical approach. Previous reports have documented the negative impact of hypertension and increased left atrial diameter on the success of pulmonary vein isolation for AF treatment (Eur Heart J 28: 836-841, 2007), perhaps highlighting the need for a more aggressive approach to achieve blood pressure control in order to prevent AF recurrence.
In this context, a recent report by Pokushalov and colleagues (J Am Coll Cardiol 60:1163-1170, 2012) addressed the question whether pulmonary vein isolation (PVI) combined with catheter-based renal denervation, a recently introduced technique that has been shown to result in significant blood pressure reduction by ablating the sympathetic nerves surrounding the renal arteries with radiofrequency energy (Lancet 376: 1903-1909, 2010), would be more efficacious in reducing AF recurrence than PVI alone. The rationale for combining these two techniques was that the improved blood pressure control and the anticipated reduction in sympathetic nerve activity following renal denervation may help to reduce the rate of AF recurrence in patients with poorly controlled blood pressure. Indeed, in a small cohort of patients with refractory symptomatic AF and resistant hypertension the authors noted a significant improvement in both blood pressure and AF recurrence in those patients in the combined therapy group (in the renal denervation group systolic blood pressure fell by 25 mm Hg and 69% of patients were AF-free whereas in the PVI-only group blood pressure was reduced by 5 mm Hg and only 29% of patients were AF-free).
While these results appear intriguing, they need to be interpreted with caution for the following reasons: (1) the sample size in this “first in man” study was small and the success rate in those patients undergoing pulmonary vein isolation without concomitant renal denervation to avoid recurrence of AF was surprisingly low. (2) it is unclear whether the reduced rate of AF recurrence in the combined treatment group is simply due to the blood pressure lowering effect of renal denervation, or whether renal denervation, perhaps via alteration of sympathetic tone, may provide benefits beyond blood pressure reduction in this scenario. To this end, a third arm combining PVI with additional pharmacologic treatment in order to achieve a similar reduction in blood pressure as was observed with renal denervation would be required. However, albeit performed in patients with well controlled blood pressure, the use of angiotensin receptor blockers has been shown to exert no effect on AF incidence (N Engl J Med 360:1606-1617, 2009) or cardiovascular events in patienst with AF (N Engl J Med 364:928-938, 2011). (3) Although a significant blood pressure reduction >10 mm Hg was achieved in the entire renal denervation group, 31% of patients remained in AF at 12 months, suggesting that renal denervation combined with PVI is still not sufficient to prevent AF recurrence in a significant proportion of these patients
Recent proof of concept studies and case reports documenting the effectiveness of catheter based renal denervation in reducing blood pressure, ventricular arrhythmias (Clin Res Cardiol 101:63-67, 2012) , left atrial diameter and left ventricular hypertrophy, and heart rate (J Am Coll Cardiol 59:901-909, 2012) highlight the importance of the sympathetic nervous system in cardiovascular disease and provide the theoretical background for much needed future studies to delineate a potential role of renal denervation in the future treatment of AF.
中文摘要:肺静脉隔离是治疗反复发作的阵发性心房颤动(房颤)的成熟方法,高血压和增大的左心房直径对肺静脉隔离的成功率有不良影响,我们需要采用更积极方法控制血压以预防房颤。
这篇文章探讨了肾脏去神经术+肺静脉隔离对房颤复发是否优于单用肺静脉隔离。联用这两种技术的理由是血压水平的改善和交感神经活性的减弱将有助于减少血压控制不良患者的房颤发作。在这项小型研究中,对难治性高血压和难治性症状性房颤患者,联合治疗显著降低了血压和房颤的复发率。
这些结果很有趣,但需要注意以下几点。首先,这项第一次在人体中进行的研究的样本量很小,而且单用肺静脉隔离预防房颤复发的成功率出人意料得低。其次,不清楚联用的效果是来自于肾脏去神经术导致的血压下降,还是由于交感神经活性改变产生的血压之外的效益。另设一组——肺静脉隔离加用药物以达到类似的血压下降幅度,将有助于回答这个问题。第三,联用组仍有31%的患者在12个月时有房颤,表明肾脏去神经术联合肺静脉隔离对预防房颤复发仍然是不够的。
近期的文献报告了肾脏去神经术对室性心律失常、左心房扩大、左心室肥厚和心率的作用,提示交感神经系统在心血管病中的重要地位,提供了研究肾脏去神经术在房颤治疗中作用的理论基础。



 京公网安备 11010502033353号
京公网安备 11010502033353号